Charles Best and Frederick Banting: The Scientists Who Discovered Insulin
It was the call that every scientist dreamed of receiving when Frederick Banting’s phone rang one October morning in 1923. It was no other than his laboratory colleague who was inquiring whether Banting had read the morning newspapers. Banting’s colleague informed him that he was being honored with the Nobel Prize in Medicine or Physiology for his discovery of insulin. However, to his dismay, Charles Best, who had played a significant role in the discovery, was nowhere to be found in the newspaper. Instead the shared honor had gone to John Macleod.
Below World History Edu explores the lives and works of Charles H. Best and Frederick Banting, the two scientists who discovered insulin. It takes readers on a story about huge egos, vicious professional rivalries, and injustices, with diabetes as its main character. But first, here is a quick look at the disease itself.

History and Major Works of Charles H. Best and Frederick Banting
The Slow Poison
Diabetes is named after the ancient Greek term “to flow,” a reference to one of its most common symptoms. For this, the 17th-century English doctor Thomas Willis gave the far more iconic nickname “the pissing evil.” However, frequent toilet trips were the least of a patient’s worries since the disease could quickly kill you over time. Having type 1 diabetes meant certain death prior to the discovery of insulin.
Patients unable to metabolize sugar from carbs in their diet were weak and malnourished until they fell into coma and later died due to the creation of poisonous chemicals known as ketones in their bodies. Even during the twentieth century, there was nothing that could be done for individuals suffering from this illness other than to starve them, which could only postpone the inevitable.
Frederick Banting
Frederick Grant Banting, born in 1891, was a surgeon in Canada with a failing practice. Banting, the youngest son of Methodist farmers from Ontario, was on the verge of entering the Methodist ministry but decided at the last minute that his true calling was medicine.
During World War I, he was a battalion medical officer in the Canadian Army Medical Corps; after being injured in the arm by shrapnel, he returned to Toronto, Canada, in 1919. Banting’s career plunged after he returned to Canada as a wounded war hero from the Western Front. He had studied medicine and planned to begin his own practice, such fantasies, however, appeared to evaporate rapidly. He found himself cooking his meals on a Bunsen burner, writing prescriptions for baby food, and unable to afford even a movie trip. Hopes of a different career as a landscape painter were quickly dashed when a local dealer mocked his innovative efforts.

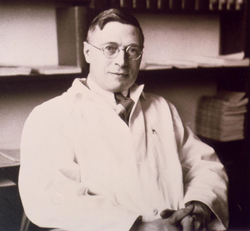
Having received the Nobel Prize at age 32, Dr. Banting remains the youngest Nobel laureate for Physiology/Medicine as of 2021. In 1934, he was knighted as a Knight Commander of the Order of the British Empire (KBE) by King George V. Image: Canadian scientist and Nobel Prize laureate Frederick Grant Banting
Bantings’ practice income was poor, forcing him to work as a demonstrator at a nearby medical school. In 1920, he was preparing a speech about the function of the pancreas when he stumbled on an article in an edition of Surgery, Gynecology, and Obstetrics titled “The Relationship of the Islets of Langerhans to Diabetes, and focused mainly on the Cases of Pancreatic Lithiasis.” That was when an idea was born.
The Meeting with John Macleod
Banting wrote down an idea for a preliminary experiment to further study the association between pancreatic secretions and diabetes when thinking about pancreatic secretions after reading the article. He brought his proposal to the attention of John James Rickard Macleod, a Scottish physiologist and expert in carbohydrate metabolism, on the advice of a colleague.
It wasn’t that Macleod wasn’t interested in what Banting had to say, instead, he was concerned that, even though Banting had a great idea, he lacked the specialized surgical abilities to carry it out. Nonetheless, he gave Banting the benefit of the doubt and arranged for him to start working with Charles H. Best, a final-year honors student. Their collaboration has since been regarded as “historic.”
The Historic Tag Team
In 1921, Banting and his assistant, Charles Herbert Best, began their investigations. Born in the United States, the brilliant scientist Charles H. Best was the son of Canadian parents. Best had just graduated from the University of Toronto with a degree in physiology and biochemistry. The scientist had been hired as a research assistant to Macleod. However, Macleod later assigned him to Banting, and the surgeon and assistant set about making history together.
Researchers in Germany and Hungary were on the brink of discovering pure insulin when their efforts were thwarted by a shortage of funds and the devastation of World War I.
Following previous investigators’ footsteps, Banting and Best proceeded to investigate diabetes using an experimental combination of duct ligation (tying off the pancreatic duct to the small intestine) and pancreatectomies (total surgical removal of the pancreas). They saw that the acini cells that create digestive secretions degeneration as a result of duct ligation leaving only the cells of the islets of Langerhans.
After completing that experiment, they concluded that diabetes did not develop in duct-ligated dogs. Pancreatectomy was used to induce diabetes during the research. Immediately after all pancreatic tissue was removed, the experimental dogs developed glycosuria and were susceptible to diabetes.
While Macleod was abroad in Europe for the summer, Banting wrote to inform him of their latest findings. But his response was disappointing. Macleod politely pointed out that some experimental results were inconsistent and lacked appropriate controls. When Macleod returned from his holidays, he informed Banting that the University of Toronto could not provide any more of his demands for increased lab space and resources. This infuriated Banting, who threatened to submit his work to another university.
Best and Banting claimed later in the year that they were keeping a severely diabetic dog alive with injections of an extract derived from the duct-ligated pancreas and prepared in saline according to Macleod’s directions. Surprisingly, this compound significantly reduced blood sugar levels in diabetic test dogs. This soon became their first scientific breakthrough.

Renowned scientist Dr. Banting began his works with biochemistry graduate Charles H. Best to understand diabetes. Best was elected a foreign member of the Royal Netherlands Academy of Arts and Sciences as well as the American Academy of Arts and Sciences in 1946 and 1948, respectively. Image: American-Canadian scientist Charles H. Best
Tension Builds as Findings are Presented
Things had deteriorated by the end of 1921, and with the final presentation approaching, Macleod believed it was now appropriate for Banting and Best to present their findings in public at a proper scientific conference. However, when Banting rose to address the American Physiological Society at Yale University that December, the audience’s reputation took its toll on his nerves. His presentation was a total disaster.
Desperate to steal triumph from the jaws of defeat, Macleod stepped in, took over, and completed the presentation. For Banting, this was a brazen coup by Macleod to deprive him of the credit for discovering insulin. To make matters worse, it had been done in front of the field’s most distinguished experts. It verified Banting’s growing worries that credit of the discovery was slipping from his grip, and he desperately needed to reclaim his authority over the discovery.
Purification of insulin and the first Human Trials
Macleod asked James Bertram Collip, a scientist in the department of physiology at the University of Toronto, to assist Banting and Best in purifying their extract. As the experimental tempo intensified, Banting and Best required vast quantities of their extract. Collip got to work refining the extract for clinical testing in humans. It was now time for human experiments, but the scientists had no participants.
A chance presented itself in 1922 when Leonard Thompson, who was 14 years, was on the verge of death from type 1 diabetes by the time his father brought him into Toronto General Hospital. Banting described the boy’s condition as poorly nourished, hair coming out with an acetone scent on his breath. One senior medical student stated unequivocally that the boy was doomed.
The test patient Thompson was given 15cc of pancreatic extract made by Best. The effect fell short of expectations. Collip continued to create ketones despite inducing a 25% decline in Thompson’s blood sugar levels, indicating that the extract had only a modest anti-diabetic impact. Far more significantly, the extract had produced a toxic reaction, resulting in the formation of abscesses at the injection site.
Thompson was injected two weeks later, and the outcome was markedly different this time. The kid got brighter, more active, looked better, and stated that he felt stronger. His blood sugar levels were significantly lower. But, probably most importantly, there were no lethal side effects this time.
The Secret Behind the Breakthrough
So, what happened during those two weeks? The answer was that the second batch of extract had been made by James B. Collip, not Banting and Best.
Collip was a trained biochemist who had been able to eliminate enough contaminants from the raw pancreatic extract to ensure that it did not induce a harmful reaction when administered. Alcohol was the key to Collip’s success. Banting and Best had utilized alcohol to clear up contaminants in their preparations, but it was Collip who really nailed the procedure of making an extract that could be used to successfully treat a patient with no side effects.
Collip had also learned that insulin might save lives but could also take them. When Collip injected healthy animals with some of his purified product, they became convulsive, unconscious, and eventually died. This was because Collip’s preparations had become so pure that they put the animals into hypoglycemic shock. This is a risk that every type 1 patient is now taught to recognize and, thanks to Collip’s work, it can be mitigated with some quick-acting sugar.
The scientists converged at the Association of American Physicians meeting in 1922. Macleod, representing the group, reported to the international medical community that they had discovered “insulin,” the anti-diabetic medication.
Canadian biochemist James Collip was a member of the science team that isolated insulin. Collip who really nailed the procedure of making an extract that could be used to successfully treat a patient with no side effects. Image: James Bertram Collip
The Nobel Prize and Controversies
Charles Banting and Macleod were awarded the Nobel Prize in Physiology or Medicine in 1923 for their discovery of insulin. The fact that the Nobel committee only chose Banting and Macleod for the award fueled even more resentment.
Banting, enraged that Macleod had been selected to share the prize with him, declared immediately that he would split his prize money with Charles H. Best. In response to Banting’s generosity, Macleod stated that he, too, would split his reward with Collip.
By 1923, insulin had been in commercial production for more than a year. Diabetic patients who received insulin shots came out of comas, resumed eating carbohydrates in moderation, and discovered they had been given a new chance at life.




























Great story. Thank you